Shoulder bursitis & evening pain
SHOULDER BURSITIS & EVENING PAIN
Shoulder pain (usually non-traumatic or of gradual onset) is the third most common cause of consultations for musculoskeletal pain by General Practitioners (1).
SHOULDER BURSITIS: A LEADING CAUSE OF EVENING SHOULDER PAIN
With many shoulder conditions there comes a point where the pain progresses from being experienced only during the day to being experienced in the evening. Many patients who I consult in clinical practice experience pain in the shoulder of an evening. Pain is experienced when they attempt to lie on the sore or injured shoulder or roll onto that side during an evening’s sleep. However many are unable to do enjoy such a simple pleasure as an uninterrupted evening’s sleep because of the pain emanating from their shoulder.
The patient will often act on their pain in seeking professional help because their evening’s sleep has become disrupted. While there are numerous structures in a shoulder that can become painful in the evening, most shoulder related evening pain indicates that the sub-acromial bursa of the shoulder has likely become a source of pain for the patient, due to its inflammation and irritation.
WHAT IS THE SUB-ACROMIAL BURSA?
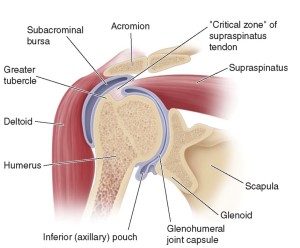
The sub-acromial bursa (also known as the sub-deltoid bursa) is often described as being a ‘fluid-filled sac’. This ‘sac’ that sits underneath the arch of the acromion process of the shoulder’s bony anatomy, the coracoacromial ligament, and the deltoid muscle. While ‘sitting’ underneath these three structures, the bursa sits on top of the tendons (supraspinatus and infraspinatus) of the shoulder’s rotator cuff. The bursa is generally enclosed with fat and is mucus like in its viscosity. See diagram:
The function of the bursa is to serve as a gliding mechanism between the rotator cuff tendons and the coracoacromial arch of the shoulder. Without the sub-acromial bursa in place, the rotator cuff tendons would be subject to excessive compressive and tensile loads which would result in degenerative rotator cuff tendons. The subacromial bursa is highly innervated by nerves that descend from the nearby neck, and is, therefore, a highly sensitive structure, prone to possible irritation and subsequent pain.
HOW DOES THE BURSA BECOME PAINFUL?
I often coach graduate physiotherapists around the concept that the shoulder is a highly complex joint that experiences a great freedom of movement. This movement comes at the cost of a less joint support. This is in comparison to say a stable knee joint or elbow joint, whereby the movement available to the joint is a lot less, yet the stability of the joint is much greater.
The subacromial bursa is often a secondary or additional source of pain for a patient experiencing shoulder pain of some other cause. Given this high degree of shoulder movement (range of motion) when something goes wrong in the shoulder, it is very common for a combination of flow on effects and subsequent shoulder pain to occur. The original injured structure (in the above example say one of the rotator cuff tendons) loss of function begins to impact on a nearby shoulder structure such as the subacromial bursa. For example, the patient’s shoulder may have initially had an acute onset of pain due to a sudden rotator cuff tendon tear, produced as an example while lifting a heavy object. When the shoulder’s movements become dysfunctional due to the aberrant stability of the now injured shoulder and damaged rotator cuff tendon, other ‘nearby’ or local shoulder structures are at risk of getting ‘banged around’ or ‘overloaded’. They, therefore, can become additional pain generators. One of the key structures that are impacted upon following the onset of dysfunctional movements after an acute shoulder injury, tends to be the sub-acromial bursa.
This example is seen in most instances of long-standing and unresolved rotator cuff tendon injuries. Subacromial bursitis can also be sequelae of acute onset tendon tears, various shoulder impingement conditions, and also traumatic sporting injuries.
In the above example of a torn rotator cuff tendon, the subacromial bursa is in effect ‘pinched’ with movements into the plane of motion either in front or to the side of the body approaching or greater than 90 degrees. In this position, the sub-acromial bursa is ‘jammed up’ and in close contact with the shoulder’s bony anatomy. This jamming up of the bursa can result in it becoming inflamed. Such inflammation of the bursa is termed ‘bursitis’. Often it will colloquially be referred to as ‘shoulder bursitis’.
Given that most shoulder injuries have multiple contributing structures including the sub-acromial bursa, a sore shoulder has been described as being like ‘shoulder soup’. That is s there is a combination of factors (or ‘ingredients’) that exist in causing the pain experienced by the patient with the sore shoulder.
HOW IS SHOULDER BURSITIS DETECTED?
There are several ways that your physiotherapist will be able to detect possible bursitis. They include:
- Reports from the patient of pain in the shoulder when sleeping on it in the evening. In this position, the bursa is ‘squashed up’ and propagates pain.
- Pain with movements in excess of 90degrees (forwards and sideways), or hand behind the back positions.
- Special orthopaedic tests: your physiotherapist will perform a variety of tests to identify the painful shoulder structures.
- Imaging: diagnostic ultrasounds, CT scans, or MRI scans of the shoulder can all detect sub-acromial bursa problems.
WHAT ARE THE SYMPTOMS OF SUB-ACROMIAL ‘SHOULDER’ BURSITIS?
Shoulder bursitis may present with the following symptoms:
- Gradual onset of shoulder symptoms over weeks or even months.
- Pain experienced on the outside of your shoulder.
- Pain that may spread down the arm extending towards the elbow or wrist.
- The pain made worse when lying on your affected shoulder.
- The pain made worse when using your arm above your head.
- A painful arc of movement – shoulder pain felt between 60 – 90° of the arm moving up and outwards.
- When the arm is by the side there is minimal pain and above 90° relief of pain.
- Shoulder pain with activities such as washing hair, reaching up to the high shelf in the cupboard.
WHAT CAN YOU DO ABOUT IT? TREATMENT OPTIONS
I tend to approach the shoulder bursitis of the patient’s that I treat in two categories: long-standing (or chronic) or more acute (short onset time).
For longer-term or chronic shoulder subacromial bursitis I tend to recommend the following course of action:
- Imaging of the shoulder if not yet performed (e.g. ultrasound imaging via a referral from their General Practitioner). Having this imaging upfront in cases of chronic shoulder pain I believe is in the patient’s best interest in optimising their recovery.
- NSAID (non -steroidal anti-inflammatory) medications (these may include over the counter or prescription based anti-inflammatory medications. I have observed that prescription anti-inflammatories result in greater reduction of patient symptoms due to the higher doses of anti-inflammatory agents. The time period for use may vary from 2- 4weeks or longer depending on history. Generally, though I view NSAD use as an initial tool to assist the client experience some pain relief and therefore commence effective physiotherapy.
- If NSAIDs have not yielded a significant reduction in the patient’s symptoms within 1 -3 weeks, I will often recommend the patient to return to their GP in order to obtain a referral for an ultrasound-guided cortisone injection. There exists a stigma around cortisone’s use due to what may be referred to as misuse and misguided use in earlier decades of musculoskeletal injury management. I will normally outline to the client that under ultrasound guidance injecting a chronically irritated bursa is ‘best practice’ and given the accuracy of the procedure, it is also safe. There may be instances whereby I recommend that the patient skips step 2 and goes straight for an ultrasound guided injection. Such cases typically include the chronic and very long-standing shoulder pain conditions. These may be due to osteoarthritis of the shoulder, or impingement of the shoulder due to bony abnormalities of the acromion process (e.g. beaked or spurred acromion process).
Injections of cortisone via ultrasound guidance have been found to be more effective in the relieving of subacromial bursa symptoms than ‘blind’ (unguided injections) (2).
- Commencement of physiotherapy. Physiotherapy can be broken down into three stages: pain –relief, the range of motion, and strength and conditioning. Each stage is not mutually exclusive; rather they are addressed and improved in an ‘over-lapping’ nature. A combination of manual (hands-on therapy) including soft-tissue releases/massage, acupuncture (dry needling), shoulder and spinal mobilisation techniques, and exercise based rehabilitation will be required. Two commonly prescribed exercises effective for sub-acromial bursitis that I give to patients are 1. The wall press click HERE, 2. Use of the Pocket Physio for the back of the shoulder click HERE.
- Referral to a shoulder surgeon may be indicated if 1-4 have not been effective. If a disciplined and effective process is undertaken by the physiotherapist and patient alike, and symptoms remain (eg the shoulder may be 80% functional or ‘good’ but pain with certain activities remains) than a referral to a shoulder specialist or surgeon may be required. This is organised via GP referral. A surgeon’s typical role in operating for shoulder bursitis is to perform arthroscopic ‘clean up’ of the irritated bursa. The surgeon may in some instances also need to remove any bony impediments from the shoulder which left uncorrected may perpetuate irritation of the shoulder’s bursa.
REFERENCES:
(1) Brox JI,Sunde P, Schroder CP, Engebretsen K, Skare O, Ekeberg OM, Juel NG. Non-traumatic shoulder pain. Tidsskr Nor Laegeforen. 2010 Nov 4;130(21):2132-5
(2) Chen, Max J. L. MD; Lew, Henry L. MD, PhD; Hsu, Tsz-Ching MD, PhD; Tsai, Wen-Chung MD, PhD; Lin, Wei-Ching MD; Tang, Simon F. T. MD; Lee, Ya-Chen MD; Hsu, Rex C. H. MD; Chen, Carl P. C. MD. Ultrasound Guided Injections in the Treatment of Sub-acromial Bursitis. American Journal of Physical Medicine & Rehabilitation: Jan 2006-vol 84 (1), pp 31-35.
PAIN-FREE. PERFORM. PROLONG
Brad Beer (APAM)
Physiotherapist, Bestselling Author of ‘You CAN Run Pain Free!‘, Founder POGO Physio