Run Pain and Injury Free – Importance of Identifying and Managing Shin Pain
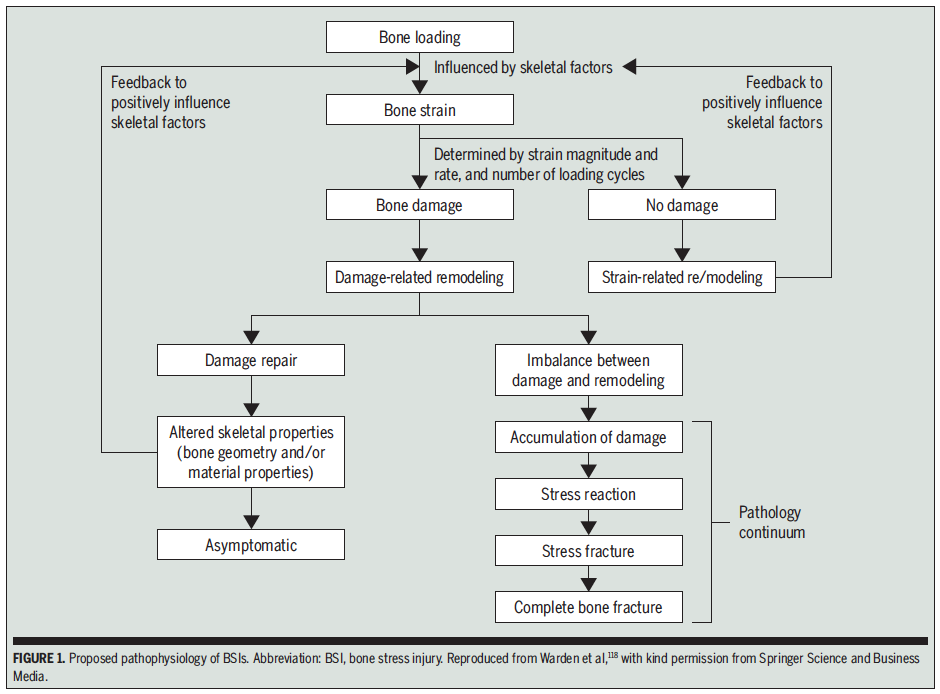
A bone stress injury (BSI) represents the inability of bone to withstand repetitive mechanical loading, which results in structural fatigue and localised bone pain and tenderness. Bone stress injuries occur along a pathology continuum beginning with stress reactions, which can progress to stress fractures and, ultimately, complete bone fractures. The occurrence of these injuries in the tibia are known commonly as ‘shin splints,’ or medial tibial stress syndrome (MTSS) clinically. Here we highlight important details in prevention and management options for BSIs in runners.
Prevalence:
Between one third and two thirds of competitive cross-country and long-distance runners have a history of BSI (1). Among these injuries approximately half occur in the tibia (MTSS), with estimated occurrence of 13-20% of runners (2). Unfortunately there can also be high rates of reoccurrence without thorough management and modification of contributing factors.
Pathophysiology:
Bone readily adapts to the loads placed upon it. Loading bone creates microdamage within the bone, which normally will be remodeled by osteoclasts (bone producing cells) to change bone density or bone characteristics. This makes the bone stronger and more resistant to loading demands. When there is an imbalance between microdamage and remodelling the pathology continuum becomes established: stress reaction to stress fracture to complete fracture (see figure 1 below).
So what leads to excess microdamage?
It is difficult to study many contributing factors for MTSS as it requires the following of a large number of runners for long periods of time. However there is evidence to suggest a number of factors can influence the development of BSI, and particularly MTSS. These may include;
- Biomechanical factors (including high ground reaction forces, increased body weight, alignment, flat feet – navicular drop, running gait kinematics – i.e your running technique)
- Training factors (including sudden increases in duration, frequency of training sessions, running intensity or addition of hills)
- Reduced muscle strength and endurance (particularly calf muscles)
- Training on hard surfaces and terrain
- Inappropriate footwear or inserts (orthoses and insoles)
Diagnosis:
BSIs often present with a history consistent with overuse injury, a gradual onset of activity-related pain. Signs and symptoms may vary depending on the point in the continuum at which the runner presents. Common symptoms include:
- Pain or tenderness along or at a single point on the tibia
- Pain with initial activity
- Pain is worse with increased limb loading, hills or hard surface running
- Pain with single log hop test.
- Stiff and tight stiff in the morning and post exercise
A thorough history and examination will be used to determine diagnosis and identify important contributing factors. Diagnostic imaging, such as a bone scan or MRI can be an additional tool to confirm assessment findings.
Management:
Specific management is variable depending on the individual presentation, point in the pathology continuum and contributing factors. Initial management will involve activity modification and managing bone loading. Manual therapy can help reduce shin discomfort as well as address identification of risk factors and graduated return to running and sport. It is vital to see a physiotherapist to help diagnose the condition and develop an individualised management program, to get you back running painfree and at your best.
Lewis Craig (APAM)
POGO Physiotherapist

References
- Warden, S. J., Davis, I. S., & Fredericson, M. (2014). Management and prevention of bone stress injuries in long-distance runners. journal of orthopaedic & sports physical therapy, 44(10), 749-765.
- Lopes AD, Hespanhol LC Jr, Yeung SS, et al. What are the main running-related musculoskeletal injuries? A systematic review. Sports Med 2012;42:891–905.
- Moen, M. H., Bongers, T., Bakker, E. W., Zimmermann, W. O., Weir, A., Tol, J. L., & Backx, F. J. G. (2012). Risk factors and prognostic indicators for medial tibial stress syndrome. Scandinavian Journal of Medicine & Science in Sports, 22(1), 34-39. doi:10.1111/j.1600-0838.2010.01144.x
- Franklyn, M., & Oakes, B. (2015). Aetiology and mechanisms of injury in medial tibial stress syndrome: Current and future developments. World Journal of Orthopedics, 6(8), 577.