Lateral Ankle Ligament Sprains Part 1
Lateral Ankle Ligament Sprains Part 1
What’s gone wrong and how do I start my acute phase rehab?
If you’re like me, at some point in your life so far, you’ve probably rolled and sprained your ankle. Whether you were running at school and rolled your ankle in that annoying pot-hole, or rolled your ankle running along the pavement passing a fellow runner, sprained ankles are annoying and frustrating. Treating a sprained ankle well and completely is essential to ensure a more chronic issue doesn’t develop.
Treating a sprained ankle well and completely is essential to ensure a more chronic issue doesn’t develop #physio #ankle Share on X
This blog post is the first of a two part blog series about lateral ankle sprains. Part one, will explore how a lateral ligament ankle sprain occurs, and how to best treat it in the acute phase. Part two of the blog post will explore how to make sure you rehabilitate your lateral ankle sprain comprehensively in the subacute phase.
What joints make up the ankle complex?
The ankle complex is made up of three key joints:
- The talocrural joint – formed by the talus and tibia and fibula. This is the true ankle joint, allowing ankle flexion and extension
- The subtalar joint – formed by the talus and calcaneum. This joint enables inversion and eversion of the ankle joint, allowing the foot and ankle joint to adapt to uneven surfaces.
- The inferior tibiofibular joint – formed by the inferior tibia and fibula. This joint has minimal movement, however, assist in load and force distribution.
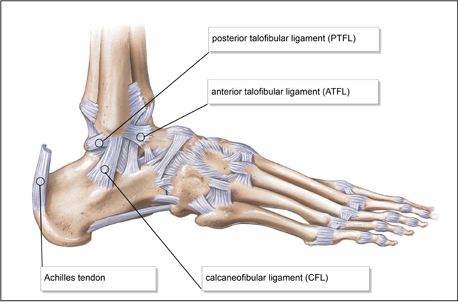
Lateral ankle ligament anatomy.
What do the ankle ligaments do?
The ligaments surrounding the ankle joints provide passive stability, limiting range of movement to provide the necessary stability required. Ligaments run from bone to bone, we don’t have to think about ‘turning them on’ to provide stability at our joints; they just automatically do (or don’t if you have poor proprioception or laxity). Our ankle ligaments are highly nerve innervated and provide feedback via proprioceptive loops to our brain automatically. These loops tell our brain where our foot and ankle are in space. Due to their high nerve innervation, they can be quite painful when sprained. The ankle ligaments unfortunately lack good blood supply, and this limits their healing capacity somewhat, making it even more important to rehabilitate them well!
What are the main ligaments involved in ankle stability?
A number of ligaments surround the ankle joints, but they can largely be categorised into two main groups:
- The lateral ligaments – including the anterior talo-fibular ligament (ATFL), the calcaneo-fibular ligament and the posterior talo-fibular ligaments. These ligaments are more commonly injured and become taut in ankle inversion and flexion. They help therefore to prevent excessive ankle flexion and inversion.
- The medial deltoid ligament – this ligament is a broad, strong, fan-shaped ligament, extending medially on the ankle and is comprised of a deep and superficial layer. Due to it’s anatomically stronger nature, it is more rarely injured. The medial deltoid ligament become taut in ankle eversion, thus becomes injured if excessive eversion forces are placed on the ankle.

Medial (or deltoid) ligament anatomy
How does a lateral ankle ligament sprain happen?
As discussed already, the lateral ligaments of the ankle are more commonly injured than the medial ligament. As a general rule the mechanism of injury for spraining the lateral ligaments is a plantar flexion (toes pointed) with inversion (foot rolling inwards) combination. The ATFL, CFL and PCL lateral ankle ligaments provide stability to limit inversion of the foot, but when the force applied to the ligaments exceeds their ability to absorb and withstand their force, over-stretching and tearing of a percentage of the fibres occurs.
The grade of the ligament sprain sustained depends upon the degree of tearing within the ligaments that occurs. Due to its anatomical arrangement, the ATFL is the most commonly sprained ligament, followed by the CFL ligament, followed by the PCL ligament. The PCL ligament is the strongest and is typically only injured in a high trauma ankle injury and if completely torn typically requires surgery to restore functional ankle stability.
The lateral ligaments of the ankle are more commonly injured than the medial ligament #sports #injury #physio Share on X
Common mechanism of injury:
Commonly, people who present with sprained lateral ligaments of the ankle report the following mechanism of injury:
- Running and landing with their foot on the edge of the pathway
- Foot landing in a pothole while running on grass
- Sudden change of direction while playing football or sport
- Landing from a jump and rolling an ankle in the landing process
What are the predisposing factors to a lateral ankle sprain?
A number of predisposing factors can be present, which may have lead to an increased risk of you sustaining a lateral ankle ligament sprain. These include:
- A past history of ankle sprains – due to prior ligament laxity and instability – typically this is clinically accepted as a risk factor, however not well proven in the literature.
- Poor running technique
- Inappropriate footwear selection
- Tight or weak calf muscle strength
- Poor ankle balance and proprioception
- Poor hip stability
- Change in training surface or playing surface
- External factors – such as the playing surface, running track quality or type of sport being played
What are the signs and symptoms of a lateral ligament ankle sprain?
The degree of signs and symptoms experienced varies significantly depending upon the degree of the ligament sprain, but usually the following occurs:
- Tenderness over the lateral ligaments on palpation.
- Loss of ankle range of pain-free motion
- Loss of end feel on specific ankle laxity testing
- Inability to walk and weight-bear
- Pain and swelling – usually worse at the end of the day
- Poor standing balance and stability
- Pain with running, kicking, calf raise and jumping activities
Acute management of acute ankle ligament sprains:
Apply the RICER principles:
Following the RICER principles immediately after ankle ligament sprain will greatly enhance healing times. The RICER principles are as follows:
- Rest – de-load the ankle ligaments by either utilising crutches or simply weight-bearing less on the ankle. If you’re walking around on a sore ankle and it’s giving you pain, there’s a good chance you’re hindering the healing process, not helping it
- Ice – Immediately after the injury icing the lateral ankle ligaments is essential to assist in reducing tissue metabolism. Crushed ice, cool packs or frozen gel packs are all useful tools. Take care to ensure you don’t give yourself an ice burn so put a layer (ie a thin towel) between the ice and your ankle.
- How long should I apply ice for?
- The evidence is still limited on what works best, but generally applying ice for 20 minutes on/20 mins off for the first 24 hours is regarded as best practice. After the first 24 hours, applying ice for 20 minutes every 2 hours is a useful protocol to follow.
- How long should I apply ice for?
- Compression – Compression with a firm bandage or Tubigrip wrap is useful in further minimizing swelling and also provides some support for the injured ankle.
- Elevation – Elevation of the injured ankle ligaments helps decrease hydrostatic pressure and therefore reduces interstitial fluid accumulation further. Ideally the injured ankle will respond best if positioned above the heart, but if sitting is required, placing the foot up on a chair is better than it staying down below the pelvis.
- Referral – Referral on to your local physiotherapist/GP or hospital depending on injury severity and pain levels is important in making sure you get started on the best management plan as soon as possible and also to make sure no further ankle damage is present (ie fractures).
When do I get an x-ray done?
The Ottawa Ankle X-ray rules are a set of guidelines, developed to help guide you when an x-ray may be required to rule out ankle fractures. The rules state that you should get an x-ray if there is pain over the malleolar area and any of the following:
- Bony tenderness over the lateral or medial malleolar area
- An inability to weight-bear immediately and over 4 steps at the time of assessment or at ED
These guidelines will help you determine whether to pursue getting an x-ray done. One literature review found that only 2% of people who were negative regarding the Ottawa Rules actually ended up having a fracture.
What does physio do in the acute/early rehab phase?
The main goals of physiotherapy in the acute rehab phase of a lateral ankle sprain are to:
- Minimise swelling accumulation at the ankle injury site
- Pain-relief
- Support the ankle via taping or utilise crutches to de-load the injury ankle ligaments
- Maintain maximal range of pain-free range of ankle motion
- Avoid further injury and irritation of sprained ankle ligaments
- Stimulate the ligament healing processes
Your physiotherapist will often utilise a combination of the following therapies in the acute phase to help stimulate and promote the fastest possible recovery from an ankle sprain:
- Soft tissue massage of the calf, plantar fascia, and surrounding ankle muscles
- Dry needling of the injured ligaments
- Gentle foot and ankle joint mobilisations
- Strapping or taping of the ankle
- Gentle Oedema massage to help reduce swelling
- Set you up with a home exercise program, aimed at improving ankle range of motion and to help get you fully recovered as soon as possible!
When do I start physio and rehab?
Ideally, your ankle rehab starts from the moment you injury your ankle, starting with applying the RICER principles as described above. Typically, the better you look after your sprained ankle in the early stages, the better and faster rehabilitation process you set yourself up for.
What not to do with an acute ankle sprain:
Avoid the following to maximise injury recovery speed:
- Avoid heat on the injured ankle ligaments – heat encourages fluid accumulation which may slow down the recovery process significantly
- Avoid alcohol consumption – this encourages increase fluid retention and blood vessel dilation which leads to more swelling
- Avoid inappropriate weight-bearing for the first few days – rest is an important part of the initial management phase, so avoid using the ankle lots until it’s relatively pain-free.
What next?
If you’ve sprained your lateral ankle ligaments make sure you see your local physiotherapist who will help devise a specific, individualised treatment plan to assist in helping you complete a full rehabilitation. Your physiotherapist will help minimise your injury time and maximise the speed of your return to doing the things you love to pain and injury free! Keep posted for part 2 of this blog series ‘Lateral Ankle Ligament Sprains Part 2 – best practice rehabilitation for ankle sprains.’
Jacob Taylor (APAM)
Physiotherapist

References:
Bachmann, L. M., Kolb, E., Koller, M. T., Steurer, J. & Gerben ter, R. (2003). Accuracy of Ottawa ankle rules to exclude fracture of the ankle and mid-foot: a systematic review. British Medical Journal, 326, 417.
Beynnon, B. D., Murphy, D. F., Alosa, D. M. (2002). Predictive factors for lateral ankle sprain: A literature review. Journal of Athletic Training, 37 (4), 376-380.
Brukner, P. & Khan, K. (2007). Clinical Sports Medicine (3rd ed). McGraw-Hill, Sydney.
Stiell, I. G., McKnight, R. D., Greenberg, G. H., et al. (1994). Implementation of the Ottawa Ankle Rules, JAMA, 271, 827-832.







There is no severity in an ankle sprain because it is always severe in nature. thank you so much for availing such a bundle of info with us.
Our pleasure.
Regards Brad Beer