13 Top Tips that will help your Proximal Hamstring Tendinopathy
Proximal hamstring tendinopathy injuries are common among distance runners, and track and field athletes. This injury can also be common in sports that involve a lot of agility such as court or team sports. However, it is not just the athletic population that can experience proximal hamstring tendinopathy. People who sit a lot, and peri-menopausal women can develop this injury. People who suffer insulin resistance have a greater likelihood of developing this injury (1).
How do you know if you have proximal hamstring tendinopathy?
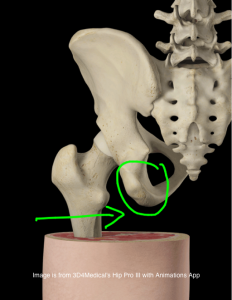
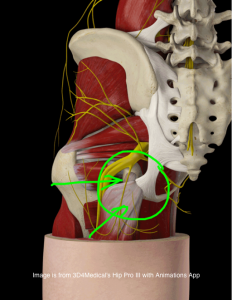
The hallmark of this condition is deep localised pain in the region of the sitting bone (ischial tuberosity) at the site of the hamstring tendon insertions (see the below diagrams for bony and tendon anatomy). The pain is characteristically aggravated by prolonged sitting, or activities such as running or squatting.
What tissue changes that occur with proximal hamstring tendinopathy
At a tissue level hamstring tendinopathy tissue will show a greater number of cells, disorganisation of the collagen fibres (building blocks of tendons), a build-up of cell ground substance, and at times nerve and blood vessel ingrowth.
My clinical insights
At any given time I am often treating half a dozen runners with a proximal hamstring injury. Like any tendon injury, progress can often be slow, and frustration levels of the injured runner can often be high. To help ensure that a runner who is experiencing pain with their proximal hamstring gets out of pain and back to their best running in the most streamlined manner possible, here are my top thirteen insights garnered through ten years of clinical experience.
Like any tendon injury, progress can often be slow, and frustration levels of the injured runner can often be high. #performbetter @pogophysio Share on X1. Get clear on the diagnosis.
Diagnosis determines prognosis. Your therapist or health professional needs to accurately diagnose your pain. Potential diagnoses in this region of pain can include: pain at the site of tendon insertion onto the sitting bone itself (enthesopathy), bone marrow oedema (fluid under the sub-chondral layer of bone), or a degree of ischio-gluteal bursitis. Pain in this area can also be referred from lower back conditions (such as vertebrae joint changes, discogenic conditions, or nerve root irritation or entrapment). The sciatic nerve can also generate pain at this region. In younger people with this condition a therapist needs to consider apophysitis, or an unfused ischial growth plate. In rare instances the posterior pubic ramus or ischial ramus may develop a stress reaction or fracture. Without a clear diagnosis being made treatment can potentially be misdirected, resulting in greater frustration experienced by the sufferer, and sadly often escalating treatment costs as the individual chases a definitive diagnosis.
Get clear on the diagnosis. Diagnosis determines prognosis. #performbetter @pogophysio Share on X2. In chronic cases I like my clients to have an MRI. This allows for exact identification of structures that may be causal of the pain, and also quantification of the degree of tissue changes. This in turn allows for an accurate prognosis for the runner. When a injured runner has a time-frame to aim for their anxiety levels, and to a degree their frustration levels typically decrease. Having a definitive diagnosis also allows for a realistic and positive expectancy to be developed by the injured runner.
3. Monitor pain levels with activity and after activity. Some pain is acceptable during and after exercise, but pain should settle within a few hours, and should not worsen over the course of the prescribed rehabilitation process. It is not uncommon for runners to be able to continue running at an easy state within pain guidelines (click HERE for a visual pain guide>>)
4. De-load the irritated tendon. For runners this can involve reducing the number of runs, removing speed work, eliminating hills from your program, or lessening the weekly volume. For track athletes this can involve the avoidance of starts, hurdles, and speed work. If you are a triathlete I suggesting continuing to ride: avoiding hills, and big gear efforts, and also getting off the time trial bike until symptoms begin to settle.
5. Don’t stretch the hamstrings. This can create a compressive force on the tendon, in effect pushing the already sensitised tendon onto the bone, delaying recovery, and increasing symptoms.
6. Sit on a cushion to help reduce compressive forces at the level of the tendon insertion onto the bone. Many runners suffering more progressed hamstring injuries experience pain with sitting.
7. Use anti-inflammatories to help settle the pain in reactive stage. Previous concerns about NSAIDs being deleterious to tendon healing less substantiated now. NSAIDs used in the early ‘reactive’ stage of tendon pain may in fact influence tenocyte (tendon cell) stimulation (1).
8. Commence isometric loading of the tendon-via your physiotherapists prescription. The exercise given to you will be dependent on your load tolerance-i.e. what you can, and cannot do within appropriate pain tolerance levels. Holds of 30-60 seconds repeated 3-4 times and up to 4 times daily may be effective in reducing pain. For an idea on isometric exercise positions click HERE>> Note: Be consistent with the completion of these exercises. As with most things in life, consistency yields great results. When it comes to corrective exercise a consistent approach, rather than a ‘perfect’ daily approach, is in my opinion superior.
9. As pain begins to settle isotonic (concentric and eccentric contractions) exercises can be added, whereby the focus is on performing them slowly. Exercises can include Nordic curls, prone leg curls, and prone hip extension. These can be completed every second day.
10. Build strength and capacity in your hip muscles. These include the gluteus maximus, medius, and deep hip rotatores. The effect of improved strength with these muscles is two-fold: less dominance of the hamstrings with running and activities, and a reduced degree of hip adduction (inwards collapsing of the thigh toward the midline) and internal rotation (inwards rotation of the hip). The net effect of this is reduced adverse load at the site of the hamstring insertion onto the sitting bone (ie region of pain). For further detailed information about developing hip muscle strength here are four great exercises you can begin with, click HERE>>
11. Some evidence exists for Extracorporeal Shockwave Therapy (ESWT). It may have a pain relieving effect, however it may also ‘flare’ symptoms (1). One study used ECSWT unit over a 4 week period, followed up at 3 and 12 months in a cohort of 20 PHT patients aged 18–25. A superior result to traditional conservative treatment was reported (1). The mechanism of effect remains unclear. For more shock wave information click HERE>>
12. Stay clear of cortisone injections into the tendon structures. This may provide a good short term outcome but poorer long term outcomes. Cortisone injections may be useful if injected around the irritated tendon (peritendon) if there are treatment plateaus, or if nerve symptoms are present.
13. PRP (platelet rich plasma injections) may provide some benefit for advanced and chronic cases, however if performed in the reactive (early) phase of symptoms, the symptoms may be exacerbated. Click HERE>> to read more about PRP injection therapies.
Lastly I often say to injured and frustrated runners who feel like they have lost hope of ever returning to enjoy their much loved running, that you have two options: stop and find another activity, or persist until you get the result. For the runners who value running as a high priority they typically persist-incurring costs of treatment along the way, but a cost that they are happy to spend in the return to their sport. Communication with your therapist is crucial. Your therapist at any given point on the journey towards recovery is there to coach you through the often times very long process of recovery. Without clear and transparent communication getting a great outcome is unlikely.
stop and find another activity, or persist until you get the result. #performbetter @pogophysio Share on XIf you have any questions or comments please go ahead and leave them below.
For further help please refer to the below resource
- Listen to tendon expert physiotherapist and researcher Associate Professor Dr Peter Malliaras discuss the rehabilitation of tendon injuries on Episode 62 of The Physical Performance Show podcast HERE>>



#runpainfree

Brad Beer (APAM)
Physiotherapist (APAM)
Author ‘You CAN Run Pain Free!’
Founder POGO Physio
References
- Proximal Hamstring Assessment and Management. Sport Health (Malliaris, P. and Purdam, C) Vol 32, Issue 1 (2014).






Thanks very much Brad. Very helpful I have a good physiotherapist but these will compliment what I am currently doing. The hardest thing I find is that the pain fluctuates and comes and goes and it is often hard to work out what you done that causes more pain or less pain! do you think it’s a good idea to do the isometric exercises despite not having too much pain at the moment pr go straight to the isotonic exercises ? also my physio is getting me to do 50 meter run-throughs about 3×10 each session to try and help build up the load on the tendon I think this is helping but it is so hard to know as improvement feels like it is so slow! I had proximal hamstring tendonopathy in the other leg last year so I think I definitely need to concentrate on those hip strengthening exercises that you provided . Thanks very much. If you have any other suggestions would be great . Still gotta get your book !
Hi Paul,
Thank you for your message. The fluctuating pain is typical of hamstring tendon injuries. The key is to manage the load and allow enough settling and adaptation time between loading cycles as the tendon is rehabilitated. I would consider doing some isometrics as a ‘warm up’ to the isotonic loading. I often prescribe this to my clients who like you are making progress, but still up and down on the journey. Hope this helps! (P.S use PROMO Code RUN25 if ordering the #runpainfreebook through the POGO website and get 25% OFF) All the best for 2017. Brad Beer
How do we distinguish between PHT and Slip disc /sciatica pain?
Have a history of slip disc & lately sciatica, but recently I have pain in the back of my thigh; most severe in the morning or when I get up after lying down
Good question and thank you.
A comprehensive and well conducted physical examination will be able to differentiate the two.
Eg slump testing will be +ve for sciatica, likley straight leg raise testing, whereas proximal hamstring tendinopathy will not be (unless sciatic nerve involvement).
To test the PHT one of the best tests is the bridge lift off test -which will normally elicit pain.
Proximal hamstring tendinopathy will also typically produce pain for the sufferer with sitting.
I hope this helps.
Regards Brad Beer
Hi Brad – I came across your article while researching my own proximal hamstring tendinopathy. I’ve been dealing with the injury since January (10 months) and was curious what exercises should be avoided? I’ve been doing a lot of “stage 2” exercises like prone ham curls and nordic ham curls every other day but haven’t made any progress. I do squat once a week to a high box just to keep the leg strength there, but have stopped doing single-leg deadlifts and regular deadlifts (I’m a lifter first, runner second). I’ve found easy things like mowing the lawn to be the most aggravating of the injury. I’ve also been playing softball and running the bases usually makes the injury flare up for a few days. The season is almost over (mowing and softball) and wanted to really focus on trying to rehab this hamstring once and for all. I did see a physical therapist for 3 months and he said that I was probably too strong already for the isometric exercises but I think that maybe I need to go back to stage 1. I can easily squat and deadlift 450+ pounds for reps so that’s why he thinks I need to focus more on direct hamstring work than isometrics.
Hi Marc,
Thanks for you comment.
Sorry to read of your ongoing tendon challenge.
The key is to allow a full day in between loading cycles: loading isotonics needs to get up to in time controlled curls single leg ideally prone hamstring machine of 0.3-0.4x body weight.
This read will help you HERE>>
Avoid any deep squats, bending FWDs at hips movements (eg mowing lawns), stretching. Check this blog and also my instagram gallery (@brad_beer) for a recent infographic I did that will help you.
Also suggest tuning into Expert edition podcast I recored with Dr Peter Malliaras HERE>>
If you get stuck I can do a SKYPE consult with you and do you up a rehab program/guide you through the key stages of rehab.
Regards Brad Beer
Thank you Brad for your reply.
I took 1 week off to try and let things settle and began a protocol of isometric exercise (5×45 second straight leg pull down with band) every other day, and single-leg prone hamstring curls (3×15 with 15 pounds) on subsequent days. Each session I’ve been adding 1 pound to the hamstring curls and every 5 pounds of added resistance I will lower the reps by 1, eventually working towards 6-8 reps with .3x body weight (roughly 55 pounds). I do squat once per week to a high box (17 inches) and have a 5 inch foam pad on the box so not to put pressure on the ischial tuberosity. I keep the reps low (no more than 5) and the intensity is around 80% of 1RM. Does this sound like a good plan? I can say that the hamstring is not very happy this week, and perhaps I’ve taken on too much at once. I am interested in going over a rehab program with you via skype. Please email me. Thanks
Hi Marc,
Thanks or the update.
Looks good but I suggest leaving out the squats on box at moment, and ensuring you do daily isometrics, every other day isotonics, and no running day after isotonic loading.
Will email you to set up call.
Speak soon.
Regards Brad Beer
Great article Brad. Can you pls let me know if massage is helpful to compliment this rehab advice? Thanks
Hi Rebecca,
Massage can be included but not over the affected tendon.
The key is to improve the tendon’s capacity which will be achieved through a progressive exercise program.
This recent blog will help you with symptom reduction-Part 2 blog to follow re exercise rehab.
HERE>>
Regards Brad